An Introduction to FODMAPs

Nobody’s digestion is perfect. And finding the foods that won’t frustrate your gastrointestinal tract is often a game of trial and error. Dealing with digestive concerns like gas, bloating, abdominal pain, diarrhea, or constipation aren’t fun. These problems may be caused by the FODMAP foods you’re eating.
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. (Saccharide is just another term for sugar.) These types of sugar can be minimized in the low-FODMAP diet some people adopt to support good digestive health.
Traditional health recommendations tell you to eat a large variety of fruits, vegetables, and whole grains. Research even shows a highly varied diet helps support a healthy gut and healthy microbiome. But no two people are exactly alike. Your diet may contain some normally healthy foods that your personal digestive system doesn’t work well with.
So, if you have digestive concerns, it might be worth limiting some of that variety in your diet. Low-FODMAP diets aim to eliminate or reduce the foods that most commonly feed into occasional indigestion and stomach discomfort.
What are FODMAPs?
To understand why you might be feeling the effects of FODMAPs in your diet, you first need a basic understanding of digestion in the gut. (Find a full recap of your digestive system here.)
After being broken down in your mouth and stomach, most of the food and liquid you eat is absorbed in your small intestine. Fiber and other waste products pass through the small intestine and into your large intestine.
The molecules that make it all the way into your large intestine become food for your microbiome. The sugars and carbohydrates that pass into the large intestine are fermented by bacteria. This fermentation process can create gas—and the accompanying feelings of bloating, cramping, and abdominal discomfort.
Due to individual digestive differences, you may have trouble breaking down and absorbing certain types of sugars and carbohydrates that others can absorb. This means more of the sugars pass into the large intestine, more fermentation takes place, and you’ll potentially feel more digestive discomfort.
The foods targeted by low-FODMAP diets are ones most frequently associated with poor digestion. They don’t need to be avoided by everyone, but some people do benefit from limiting or eliminating certain high-FODMAP foods.
The Chemistry of FODMAPs
As you learned above, FODMAP is an acronym for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. If you know the basic chemistry of carbohydrates, then you might be worried this is a far-reaching diet with a goal of eliminating all carbohydrates in your diet. But that’s not the case. A low-FODMAP diet only limits the intake of specific types of sugars within these carbohydrate categories.
For example, sucrose, lactose, and maltose are all disaccharides commonly found in the diet. Only fructose is limited in a low-FODMAP diet. So, you don’t need to worry about reducing all disaccharides in your diet.
These are the specific molecules targeted within each category of a low-FODMAP diet:
- Fermentable oligosaccharides (polysaccharides): fructans and galactooligosaccharides
- Disaccharides: lactose
- Monosaccharides: fructose
- Polyols: sorbitol, mannitol, and maltitol
You’ll discover your individual needs vary. For example, some fermentable oligosaccharides may need to be eliminated for a successful low-FODMAP diet, while the disaccharides and polyols foods can still be eaten, just in small amounts.
Unlike the other molecules targeted by a low-FODMAP diet, fructose isn’t limited to a threshold amount. Instead, it is limited in relationship to the amount of glucose you eat. That’s because glucose, when eaten together with fructose, helps increase the absorption of fructose in the small intestine.
When fructose is eaten alone or too much is eaten in relationship to glucose, then it will pass into the large intestine. Once in the large intestine, then fructose can cause some of the same problems as the other FODMAP molecules.
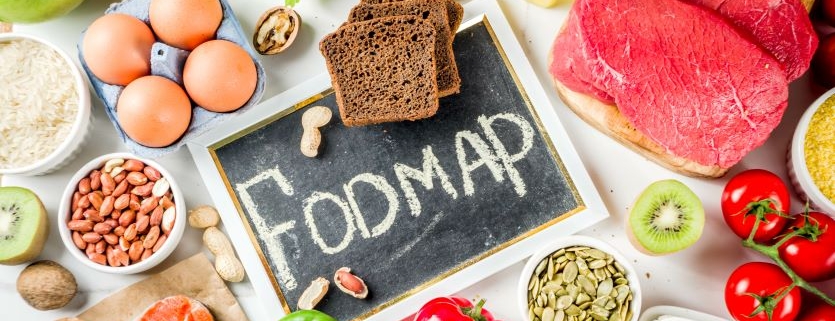
High and Low FODMAP Foods
A simple online search for “FODMAP foods” will help you find lots of lists and charts of foods to avoid or include in your diet. Below you will find a short sample list of some high-FODMAP foods (to avoid or limit), and others that are low (less likely to cause problems) in FODMAPs.
- Fructans and galactooligosaccharides
- High: wheat, rye, barley, onion, garlic, artichoke, asparagus, Brussels sprouts, cauliflower, legumes
- Low: corn, rice, quinoa, potatoes, bell pepper, cucumber, green beans,
- Lactose
- High: milk, yogurt, sour cream, ice cream
- Low: lactose-free milk, almond milk, hard cheeses
- Fructose
- High: pears, apples, watermelon, honeydew, papaya, star fruit, fruit juices, agave nectar
- Low: blueberries, strawberries, oranges, pineapple, cantaloupe, kiwi
- Polyols
- High: apples, apricots, avocados, foods sweetened with honey, sorbitol, mannitol, or maltitol
- Low: dark chocolate, table sugar, maple syrup, brown sugar
Implementing a FODMAP Diet
Not everyone will benefit from avoiding FODMAP foods. But if you decide to try a low-FODMAP diet, it’s best to work through the list of foods systematically. It’s unlikely that all high-FODMAP foods are causing you problems.
Where possible, keep as many foods and as much variety as you can in your diet. The three-step approach below will help you find out which foods may be causing problems for you. Then you know which foods you can continue to enjoy.
1. Elimination and Restriction
The best way to start is by restricting or eliminating as many high-FODMAP foods as possible. After sticking to this strict diet for a few weeks, hopefully your digestive system will feel better.
If symptoms still haven’t improved, you should work with your doctor or dietician to develop a personal plan for you and look at foods outside the FODMAP list.
2. Reintroducing Foods
If the FODMAP foods elimination has helped, it’s time to start reintroducing some options you eliminated from your diet. Reintroduce foods one at a time, and only in small amounts.
By testing out foods one at a time, you will learn which ones are safe for you to eat, and which ones need to be either eliminated or only eaten in very small amounts. After testing out a food, wait one or two days to feel how you tolerate it.
Take your time with the reintroduction phase. You’re going to be tired of eating a restricted diet and anxious for some freedom in your food choices. If you try too many FODMAP foods at once or don’t wait enough time between testing new foods, then you won’t know which choices are responsible when problems arise again (and they probably will).
There may be times when you need to go back to step one and spend a couple of weeks with a more restricted diet, just to let your GI system settle down again. Then you can start testing new foods again.
3. A Personalized Diet
Just like the FODMAP foods lists and charts you’ll find online, it’s probably worth making your own list. It will help you clearly define which foods to avoid, limit, and can be safely eaten.
By following this process of elimination and reintroduction, you may even find foods that aren’t on traditional low-FODMAP lists. This will also help create a very personalized diet.
A low-FODMAP diet requires patience to figure out, and it isn’t a magic solution that will solve all your digestive-health concerns. But it is a tool that can help you on a path to better digestion, while still includes a beneficial variety of healthy foods in your diet.